The appearance of cone-shaped flesh-colored growths in the genital area causes concern, which is completely justified, because the health of the genital area is an important factor for the general physical and moral well-being of a person.
The growth of these warts causes discomfort, interferes with normal sex life, and can cause serious health problems. If the integrity of the condylomas is broken, an infection may occur and turn into a malignant form. Therefore, the desire to get rid of such phenomena is understandable and natural.
causes of occurrence
The cause of papilloma warts is the human papillomavirus. This virus contains a specific set of DNA that successfully integrates into the cells of the human body and causes them to change their development cycle, shape and structure.

According to the International Classification of Diseases ICD-10, human papillomavirus B97. 7 codes. Anogenital warts of venereal nature A63. Code 0 is assigned.
There are different strains of this virus, each of which causes specific wart papillomas. The type of virus determines the course of the pathological process, symptoms, location and severity of the disease.
Strains fall into two main types:
- Skin with a dominant appearance in the skin layer;
- Mucous membrane formed in the mucous epithelium of the genitals, oral cavity, etc. b.
In addition, types of papillomaviruses differ depending on the risk of damage to the oncogenic process: oncogenic, moderate oncogenic and non-oncogenic.
Often, several different strains are present in an infected person's body at the same time.
Routes of infection and risk factors
There are several ways for the pathogen to enter the body:
- "vertical" transmission. The transfer of an infectious substance from mother to child during pregnancy is called this. It is not yet known whether the infection occurred prenatally or directly during childbirth, but it is undesirable to perform a cesarean section on a mother infected with papillomavirus. Cesarean section papillomas inside the birth canal are selected only in case of bleeding.
- Sexual way.An infectious agent can enter the body during vaginal, oral or anal sex. The pathogen is also transmitted through saliva during kissing. Using a condom during sex does not guarantee protection against the virus, but it does reduce the chance of transmission.
- Household road.The mechanism of transmission of this disease is very rare. Infection can be through contact with the patient's personal belongings. Because the virus is present in saliva and urine, it can be spread by sharing someone else's dishes, shared towels, personal hygiene products, toilet bowls, or baths.
The method of infection is mainly determined by the age of the person: in infants, with high confidence, it can be determined that the infection came from the mother, and for older children, it can be determined through contact and household activities. From the age of 17, it is most often transmitted sexually.
According to statistics, the human papillomavirus is present in the body of more than half of the sexually mature population, but in most cases it is invisible and in the form of carriage.
The peak of the disease occurs at the age of 17 to 25 years. This is due to the maximum sexual activity and the high sensitivity of the epithelium to the organs of the genitourinary system.
Predisposing factors that increase the likelihood of the disease:
- early onset of sexual activity;
- frequent change of sexual partners;
- age up to 25 years;
- sexual intercourse with persons who previously had human papillomavirus or other sexually transmitted diseases;
- pregnancy;
- imbalance of intravaginal flora;
- any chronic disease;
- endometriosis;
- therapy with cytostatic or glucocorticosteroids;
- overweight;
- disorders of the thyroid gland and disorders of insulin production;
- hypovitaminosis.
Frequent stress and failure to observe the principles of personal hygiene increase the possibility that the infection will enter the active phase after entering the human body.

After being introduced, the virus spreads throughout the body through the blood, attaches to cells, enters their structure, and combines its DNA with the cell's DNA. Then the affected cells begin to actively grow and divide, resulting in the formation of condylomas.
Ways of development
The virus does not cause any symptoms for a certain period of time after entering the human body.
The course of the disease is carried out according to the following algorithm:
- Secret season. At this stage, the infected person does not know the presence of an infectious agent, because there are no clinical manifestations. However, at this stage, a person is already contagious and can infect their partner through sexual intercourse. This latent period can last from 2-3 months to several years.
- The onset of the disease occurs when the virus multiplies sufficiently in the body or when the protective mechanisms of the immune system decrease. During this period, the first symptoms appear.
- Active development with increasing symptoms.
The further course of events is developing in one of the following directions:
- self-healing with the complete disappearance of papilloma warts (usually observed after the end of pregnancy);
- slow progress and stunted skin growth;
- active dynamics of papillomas: increase in shape, size, number and merging of closely located groups;
- destruction of malignant growths.
Types of condylomas
There are several conventional types of condyloma papilloma:
- exophytic- with preferential growth outside the upper surface of the skin or mucous membrane;
- endophytic- with a dominant growth in the structures of the skin, so it is not noticeable during visual inspection;
- Buschke-Levenshtein knowledge- characterized by rapid growth rates, large sizes and frequent recurrences after a course of treatment. In this form, both the outer growth and the deep inner layers of the soil are damaged.

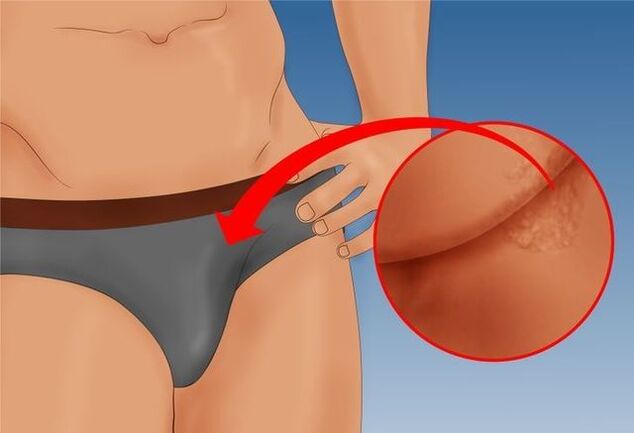
The shape of a genital wart can have a thin or wide base. If the stem is thin, the tip may be sharp or club-like. Papillomas with a wide base are very rare. The color of all such growths is close to the color of the skin: from flesh to pink. The surface can be soft or covered with a layer of keratin.
Warts can appear alone or in nodule-like groups. Sometimes the size of several such groups reaches 1, 5 cm. When several groups join together, structures similar to cauliflower florets or rooster combs are formed. These growths make it easier to detect the disease on examination.
Single growths usually do not cause as much discomfort as large elements. In rare cases, they break and bleed a little.
Larger formations are more problematic: they may become moist, bleed, and worsen due to secondary infection taking root in the affected areas.
Symptoms
The first symptoms appear shortly after the end of the latent period, which lasts several weeks.
The appearance of condylomas is as follows:
- the skin becomes slightly red and itchy;
- rash appears in the form of blisters or small bumps on the skin or mucous membrane;
- tubercles gradually grow to 1-1. 5 centimeters in length;
- New rashes appear nearby, which also turn into condyloma papules.
Localization depends on the specific strain and the site of entry of the pathogen into the body:
- external genitalia;
- anal zone (anogenital papillomas);
- in the urethra;
- in the cervix;
- in the epithelium of the mouth (on the cheek surfaces, tongue and inside the lips).

The clinical picture may vary in each specific case depending on the individual's health status. Small warts have no other symptoms.
The following symptoms, accompanied by a higher course, are observed:
- itching or burning at the site of the rash;
- sense of a foreign object in the zone;
- moisture in the area of tumors;
- unpleasant odor from the area where the warts are located.
All the above symptoms are aggravated by physical activity, long walking or running.
In severe cases, fatigue, weakness, signs of intoxication, prolonged headache, fever and temperature rise are observed.
Symptoms in men and women have some differences. This is due to anatomical differences and sexual behavior characteristics.
Manifestations in men
In men, condylomas usually affect the testis, groin, lobe and various structural parts of the penis: head, body, frenulum and foreskin, coronary groove. Papillomas localized near the urethra have a bright red color, and this localization often causes bifurcation or scattering of the flow during urination.
If the rash is located at the exit of the rectum, then there may be severe pain during bowel movements and blood in the stool. This often leads to a reflexive fear of defecation, which leads to occasional constipation and sometimes hemorrhoids.
There is often a dull ache in the lower abdomen, burning and pain during intercourse, and when urinating.
Prolonged infection lowers a man's immunity and makes him vulnerable to respiratory diseases, which are more difficult to treat than usual.
Appearances in women
In women, the most common places where papillomas appear are the perianal zones, where humidity and temperature are constantly increasing: the epithelium of the clitoris, the labia, the opening of the vagina and the opening of the urethra. If an infection occurs during anal sex, a growth ring may form around the anus.
Large growths often become secondary infections, causing a strong odor, bleeding, ulceration, and severe pain to the touch. There is irritation and severe discomfort when walking.
In 50% of women, white elements appear on the cervix, which are detected during a routine colposcopy, before which they are treated with acidic disinfectants that increase the white color of condylomas.
In some cases, all the growths are located in the mucous membrane of the internal genitals of a woman, so she does not notice it until she comes to a scheduled visit to the gynecologist. This is often the reason why treatment is started later than in men.
Often, women experience discomfort due to the presence of formations in intimate places, which forces them to refuse sex.
Papillomas are rare, and in very rare cases - on the pubis, thighs, neck or face.
Features of condylomatosis during pregnancy
If condylomatosis is treated, pregnancy should be planned no earlier than a few months. If a woman takes antiviral drugs during therapy, the period of rejection of pregnancy will be extended. After a successful treatment and an observed interval, you can become pregnant safely.
If the disease was detected during pregnancy, it is recommended to wait for treatment until all the organs of the child are already formed. Treatment after 28 weeks does not cause fetal development disorders.
The causes of condylomatous warts in pregnant women include a standard decrease in immunity, increased stress on the body, and significant hormonal changes.

If the papillomas are located on the external parts of the genitals or in the perianal zone and do not cause discomfort, then the issue of treatment can be postponed until the birth of the child. However, if you experience rapid growth, enlargement, and severe pain during adulthood, you should immediately consult a doctor. Sometimes, with a high speed of formations, their loosening is observed, which can lead to the bursting of the sheath.
This disease, as a rule, does not affect the formation of the fetus, but its influence extends to the state of the mother and the birth process. If other infections are present, there is often a risk of premature birth.
If condylomas are damaged during the passage of the fetus through the birth canal, this often leads to infection of the baby and condylomatosis of the larynx in the neonatal or thoracic period. Therefore, the presence of significant papillomas in the birth canal is a direct indication for caesarean section.
If necessary, the growth is removed during pregnancy, and then the tissue is sent for histology to check its benign nature.
It is not allowed to use the methods of traditional medicine to get rid of condyloma during pregnancy, because it can lead to the destruction of harmful cells into harmful cells without giving a positive result.
Structures that do not cause discomfort during pregnancy disappear on their own within a few months after childbirth, without treatment, as the woman's hormonal balance normalizes.
Diagnostics
If the patient notices symptoms reminiscent of human papillomavirus, he should consult a gynecologist, urologist or venereologist.
First of all, the specialist conducts a survey to clarify the following points:
- the time of detection of the first symptoms of the patient;
- possible causes of infection;
- The dynamics and development of the disease is up to the doctor.
After that, a clinical examination is carried out, during which the specialist determines the location, intensity, size and condition. For women, an additional colposcopy (examination of the private genitals with magnification) or extended colposcopy (a similar procedure performed with an acetic acid solution) is performed.
To make an accurate diagnosis, the doctor prescribes the following additional tests:
- PCR diagnostics, allows to find and quantify the pathogen from scrapings of the epithelium of the affected areas (also allows to determine the strain of the virus);
- anoscopy- visual inspection of the area near the anus with magnification;
- cytology and histologyfragments of structures to identify atypical cells or tissues;
- growth biopsyfrom epithelial tissues for microscopic examination of tissue structure;
- Determination of antibody titerthis virus;
- to pleasefrom the cervical canal and cervix for microscopic oncocytology.

If necessary, consultations with a dermatologist or proctologist are scheduled. If the diagnosis is made in a pregnant woman, it is necessary to consult an obstetrician-gynecologist.
After receiving all the necessary information, the specialist will choose therapy and individual tactics for complete relief from the disease.
To treat
Often, people with condylomatosis avoid going to medical facilities and choose therapy themselves, preferring local drugs that can eliminate the visible manifestations, but do not cure the organism of the infection, but transfer it to the latent stage. Such treatment almost always leads to relapse. Therefore, the final cure requires a comprehensive approach, which can only be determined by a specialist.
Treatment is carried out in the following directions:
- remove growths;
- fight against viruses;
- strengthen the patient's immunity.
All methods used to fight genital warts are divided into radical and therapeutic.
Radical methods
Such methods are chosen if it is necessary to quickly eliminate external manifestations or if condylomas are localized on the cervix of women.
The following methods are used for removal:
- Surgical excisionCreation using a scalpel under local or general anesthesia. The incision is sutured with surgical sutures. Despite the fact that this method is considered classic, it often leads to postoperative bleeding and long-term recovery in the hospital, so in the last case, surgical removal is used less and less.
- Cryodestruction with liquid nitrogen.This method is relatively cheap and safe, does not require anesthesia or anesthesia. After freezing, the protein of the formations is destroyed, the nodules dry up and fall off. After a few weeks, there will be no scars or scars left on the treated area.
- Laser removal.Despite its safety and high efficiency, the method requires anesthesia and is characterized by a high cost, so it is prescribed if other methods cannot be used. Under the influence of the laser beam, the structure of the growth stem is destroyed. After cauterization, the condyloma is deprived of nutrition, which leads to its necrosis and the scab disappears within a few days. Many scars remain after laser treatment.
- Electrocoagulation.The method is cheap, but very painful, so it requires local anesthesia. The genitals are subjected to high temperature, during which the papillomas are cauterized. The scabs will fall off on their own after a few days, leaving behind scars.
- Radiosurgery.Currently, this is the most high-tech, fast and effective method, which determines its high price. With the help of high-frequency radio waves, genital warts are painlessly removed in 15-30 minutes. After such removal, there is no bleeding, healing occurs within a day, after which no traces remain on the skin.
- Chemical disposal.This method is only suitable for small devices without multiple connections. Special strong substances are used, which leads to the death of growth cells. These products are based on high concentrations of acids or alkalis that cause local chemical burns.
If we limit ourselves to radical methods of combating condylomatosis, recurrence of condylomas occurs in every third case.
Drug therapy
A comprehensive approach includes the destruction of harmless structures, getting rid of the virus in the body and improving the immune status. Therefore, drug treatment includes the use of such drugs:
- Pharmacy productsFor wart necrosis, it is acceptable for home use. This product should be applied to warts for several days. If the drug comes into contact with healthy tissues near the growth site, a deep chemical burn will occur, so the drug should be used very carefully. After daily applications, take a short break of several days. If the branch does not fall, then the course is repeated. Pharmaceutical products that cause plant necrosis include solutions and oils.
- Anti-viral agents.They can be for local or systemic use.
- Immunomodulatorsto improve immunity.
In addition, systematic intake of multivitamin complexes, a special diet and a healthy lifestyle are prescribed to improve the body's defenses.
After treatment, immunity against condyloma is not formed, so re-infection from a previous sexual partner is possible.
Possible complications
If condylomatosis is not treated for a long time, the following complications appear:
- Addition of bacterial infection to damaged condylomatous papillomas, which causes purulent formations, balanoposthitis, and ulcers in the perianal zone.
- Viral-bacterial urethritis occurs when it grows in the urethra, causing urinary problems, urinary retention, and urinary tract infection.
- When large structures are localized in the anus, hemorrhoidal bleeding and paraproctitis appear.
- Genital warts can affect a person's sex life and lead to withdrawal from intercourse. All this often leads to depression and psychological problems.
- Cervical erosion and dysplasia may occur in women.
- The biggest risk is the risk of benign tumors becoming cancerous (cancer of the head of the penis or cervix).
Preventive measures
Prevention of condylomatosis is divided into specific and general.
Specific preventive measures include vaccination with the new tetravalent vaccine. These vaccines do not work against all strains of human papillomavirus, but they are effective against the most dangerous of them, which cause cervical cancer. Vaccination is carried out from the age of 11 and is repeated three times.
Non-specific prevention is similar to measures specific to many sexually transmitted diseases:
- use of barrier contraceptives;
- maintain personal hygiene at an appropriate level;
- regular sexual partner;
- regular examination by a gynecologist or andrologist;
- timely treatment of diseases of pelvic organs;
- Quitting alcohol and smoking.
In addition, stress, physical fatigue, hypothermia and various factors that weaken the immune system should be avoided. A healthy diet, good health, and proper sleep can prevent genital warts.














































































